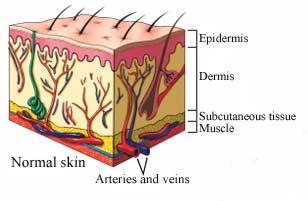
Skin Anatomy
The skin plays a crucial part in fluid and temperature regulation of our body. It also serves as a protective barrier against bacteria and viruses. If enough skin area is damaged, the ability to function as a barrier can be lost.
Burn Classifications
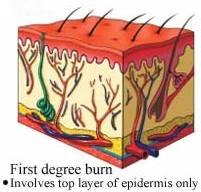
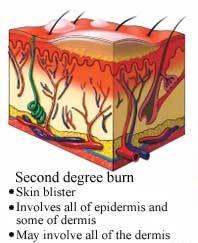
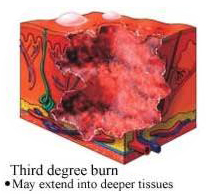
The amount of damage that a burn can cause depends upon its depth, how much of the bodys surface area it involves, and its location.
Depth
Fouth degree: These burns extend beyond all three layers of skin and deep into the muscle tissue or bone. Fourth degree burn injuries often cause a complete loss of function in the burned area. They require tissue removal or amputation.
Burns may not remain static and can mature to the next level of burn classification. Burns that extend deeper than the epidermis may cause permanent injury and scarring and not allow the skin in that area to return to normal function.
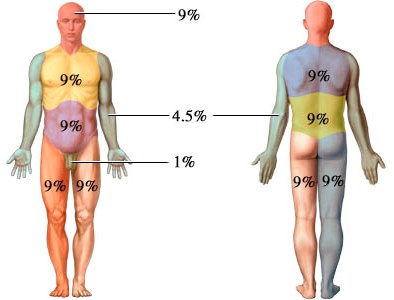
Area
An alternative method for infants, youths and small areas on adults is to compare the burn site to the size of the patient's palm, which equates to approximately 1% of the body surface area. For example, if a burn area is the size of (5) palm surfaces, the burn would be roughly 5% of the body surface areas.
If more than 15%-20% of the body is involved in a burn, significant fluid may be lost. Shock may occur if inadequate fluid is not provided intravenously. Victims with burns involving less than 20% of their body should do well, but those with burns involving 50% or higher have a greater mortality risk, depending upon a variety of factors, including underlying medical conditions and age. As the percentage of burn surface area increases, the risk of death increases as well.
Location
Burn location is an important consideration. If the burn involves the face, nose, mouth or neck, there is a risk that there will be enough inflammation and swelling to obstruct the airway and cause breathing problems.
If there are circumferential burns to the chest, as the burn progresses, the tissue involved may not allow enough motion of the chest wall to allow adequate breathing to occur. If circumferential burns occur to arms, legs, fingers, or toes, the same constriction may not allow blood flow and put the survival of the extremity at risk. Burns to areas of the body with flexion creases, like the palm of the hand, the back of the knee, the face, and the groin may need specialized care. As the burn matures, the skin may scar and shorten, preventing full range of motion of the body area.
First Aid for burns
The two major aspects to address in burn first aid are pain control and infection control.
NEVER put ice on a burn as ice is a vasoconstrictor and burns do need blood flow.
Heat burns
Major burns (second and third degree burns)
- Do not remove burned clothing. However, make sure the victim is no longer in contact with smoldering materials.
- Keep the victim warm and still.
- When possible elevate the burned body part or parts above heart level.
- Cover the area of the burn. Use a cool, moist, sterile bandage; clean, moist cloth; or moist cloth towels.
- DO NOT use cold water on the victim; doing so could cause a drop in body temperature (hypothermia) and deterioration of blood pressure and circulation (shock).
- Burns of the face, hands, and feet should always be considered a significant injury
- Call 911 or activate the emergency response system in your area if needed.
- Get a tetanus shot. Burns are susceptible to tetanus.
Minor burns (first degree burns or second degree burns involving a small area of the body)
- Gently clean the wound with cool water.
- Cool the burn. Hold the burned area under cool (not cold) running water until the pain subsides. If this is impractical, immerse the burn in cool water or cool it with cold compresses. Cooling the burn reduces swelling by conducting heat away from the skin.
- Cover the burn. Use a nonstick or non-adherent dressing. You do not want to use gauze. Telfa is an excellent choice along with a loosely bound wrap. Ace wrap works well over that. Wrap the burn loosely to avoid putting pressure on burned skin. Bandaging keeps air off the burn, reduces pain and protects blistered skin.
- Rings, bracelets, and other potentially constricting articles should be removed (edema, or swelling from inflammation may occur and the item may cut into the skin).
- The burn may be dressed with a topical antibiotic ointment like Bacitracin or Neosporin. Silvadene (silver sulfadiazine) topical is the preferred agent for most burns. Be advised that around 10-12% of the population is allergic to Neomycin which is found in Neosporin, as well as triple antibiotic ointment.
- Take an over the counter pain reliever. These include aspirin, ibuprofen (Advil, Motrin, others), naproxen (Aleve) or acetaminophen (Tylenol, others). Use caution when giving aspirin to children or teenagers. Though aspirin is approved for use in children older than age 2, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin.
- Don't apply egg whites or butter on the burn. This could cause infection.
Blisters - If you are greater than 24-48 hours from medical attention, leave the blisters on. They make great protective barriers and help prevent infection. Urgent care clinics will routinely debride the blisters since all wounds need air to heal, and after debridement, topical antibiotic ointment can be applied.
Electrical burns
Victims of electrical burns should always seek advanced medical care. Treat the same as a major burn until emergency service arrives. Not only the flesh may be affected, some internal organs could be damaged as well.
Chemical burns
Identify the chemical that was involved.
Victims with chemical burns to their eyes should always seek emergency care.
Contact the Poison Control Center in your area or your local hospital's Emergency Department. The United States National Poison Hotline is 1-800-222-1222. You will be automatically linked to the nearest poison control center. Many chemical burns may be treated with local wound care. Some chemicals can cause life- and limb-threatening injuries and need emergent intervention.
Radiation burns
Victims of "Beta burns" should always seek advanced medical care.
Radiation burns should be covered by a clean, dry dressing as soon as possible to prevent infection. Wet dressings are NOT recommended. The presence of combined injury (exposure to radiation plus trauma or radiation burn) increases the likelihood of generalized sepsis. This requires administration of systemic antimicrobial therapy.