Types
HA-MRSA
Most MRSA infections occur in people who've been in hospitals or other health care settings, such as nursing homes and dialysis centers. When it occurs in these settings, it's known as health care-associated MRSA (HA-MRSA). HA-MRSA infections typically are associated with invasive procedures or devices, such as surgeries, intravenous tubing or artificial joints.
CA-MRSA
Another type of MRSA infection has occurred in the wider community - among healthy people. This form, community-associated MRSA (CA-MRSA), often begins as a painful skin boil. It's spread by skin-to-skin contact. At-risk populations include groups such as high school wrestlers, child care workers and people who live in crowded conditions.
Causes
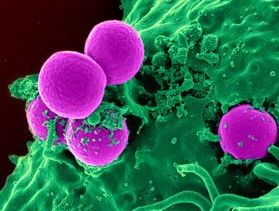
About one in four healthy people are colonized by staphylococcus bacteria. Those who are colonized have the bacteria present in their skin and nasal passages, but the presence of the bacteria doesn't make them ill. Historically, most staph was sensitive to beta-lactam antibiotics, such as penicillin, methicillin, and ampicillin. Some strains of staph developed resistance to beta-lactam antibiotics.
It is estimated that 2 percent of the population now carry a strain of staph that is resistant to beta-lactam antibiotics. Most of the staph infections that now occur in hospitals are caused by MRSA. Although aggressive infection control measures have decreased the incidence of HA-MRSA, the incidence of CA-MRSA is increasing.
Symptoms
MRSA may progress substantially within 24-48 hours of initial topical symptoms. After 72 hours, MRSA can take hold in human tissues and eventually become resistant to treatment. Within a few days, the bumps become larger and more painful; they eventually open into deep, pus-filled boils.
Most MRSA infections are skin infections that are red, swollen (fluid-filled) and painful to touch. The lesion may resemble an infected spider bite. Typically, there is yellow or white center and a central head. Pus and other fluids may drain from these lesions.
Early stages:
- Cellulitis (infection of the skin or the fat and tissues that lie immediately beneath the skin, usually starting as small red bumps in the skin with some areas resembling a bruise)
- Boils (pus-filled infections of hair follicles)
- Abscesses (collections of pus in or under the skin)
- Sty (an infection of an oil gland of the eyelid)
- Carbuncles (infections larger than an abscess, usually with several openings to the skin)
- Impetigo (a skin infection with pus-filled blisters)
- Rash (skin appears to be reddish or have red-colored areas)
Advanced stages:
- Fever
- Chills
- Low blood pressure
- Joint pains
- Severe headaches
- Shortness of breath
- Large body rash
Treatments and drugs
Both health care-associated and community-associated strains of MRSA still respond to certain antibiotics. In some cases, antibiotics may not be necessary. For example, doctors may drain a superficial abscess caused by MRSA rather than treat the infection with drugs.
Transmission
There are two major ways people become infected with MRSA.
- The first is physical contact with someone who is either infected or is a carrier (people who are not infected but are colonized with the bacteria on their body) of MRSA.
- The second way is for people to physically contact MRSA on any objects that have been touched by a MRSA-infected person or carrier.
Normal skin tissue in people usually does not allow MRSA infection to develop; however, if there are cuts, abrasions, or other skin flaws MRSA may proliferate.
Risk factors
HA-MRSA
- Being hospitalized. MRSA remains a concern in hospitals, where it can attack those most vulnerable older adults and people with weakened immune systems.
- Having an invasive medical device. Medical tubing such as intravenous lines or urinary catheters can provide a pathway for MRSA to travel into your body.
- Residing in a long-term care facility. MRSA is prevalent in nursing homes. Carriers of MRSA have the ability to spread it, even if they're not sick themselves.
CA-MRSA
- Participating in contact sports. MRSA can spread easily through cuts and abrasions and skin-to-skin contact.
- Athletes who share equipment, towels, or razors
- Living in crowded or unsanitary conditions. Outbreaks of MRSA have occurred in military training camps, child care centers and jails.
- Homosexual men have a higher risk of developing MRSA infections.
Due to a high public awareness of the virus, efforts at vaccination of domestic animals and curtailment of feral populations, and availability of postexposure prophylaxis, incidents of rabies in humans are very rare. A total of 49 cases of the disease was reported in the country between 1995 and 2011; of these, 11 are thought to have been acquired abroad. Almost all domestically acquired cases are attributed to bat bites.
Prevention
HA-MRSA
In the hospital, people who are infected or colonized with MRSA often are placed in isolation as a precaution to prevent the spread of MRSA. Visitors and health care workers caring for people in isolation may be required to wear protective garments and must follow strict hand hygiene procedures. Contaminated surfaces and laundry items should be properly disinfected.
CA-MRSA
Wash your hands. Careful hand-washing remains your best defense against germs. Scrub hands briskly for at least 15 seconds, then dry them with a disposable towel and use another towel to turn off the faucet. Carry a small bottle of hand sanitizer containing at least 62 percent alcohol for times when you don't have access to soap and water.
Keep wounds covered. Keep cuts and abrasions clean and covered with sterile, dry bandages until they heal. The pus from infected sores may contain MRSA, and keeping wounds covered will help keep the bacteria from spreading.
Keep personal items personal. Avoid sharing personal items such as towels, sheets, razors, clothing and athletic equipment. MRSA spreads on contaminated objects as well as through direct contact.
Shower after athletic games or practices. Shower immediately after each game or practice. Use soap and water.
Sanitize linens. If you have a cut or sore, wash towels and bed linens in a washing machine set to the hottest water setting (with added bleach, if possible) and dry them in a hot dryer. Wash gym and athletic clothes after each wearing.