Rabies is a zoonotic disease that affects the nervous system and causes encephalitis and, if no vaccine is administered, almost always results in death. The virus that causes rabies is Lyssavirus (Lyssa is the Greek goddess of madness, rage, and frenzy). This is an ancient disease having been documented for almost four thousand years. It has always been associated with rage and violence in the afflicted. The word rabies is derived from the Latin word rabies, which meant "madness or rage."
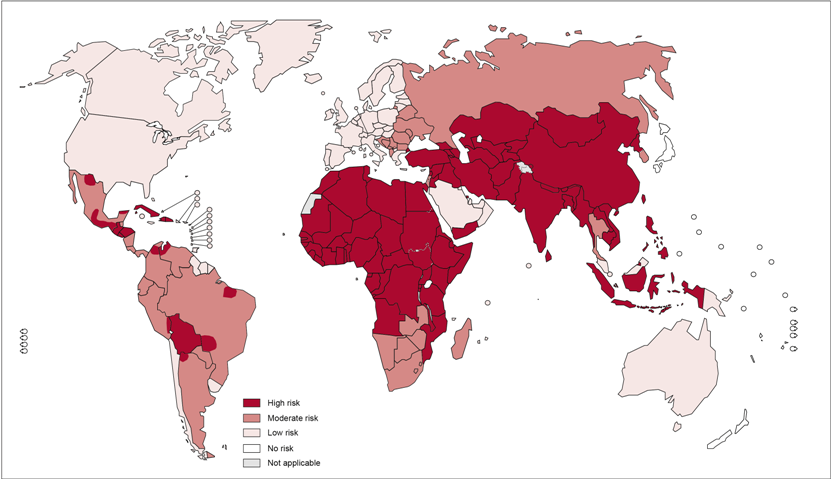
Rabies causes about 26,000 to 55,000 deaths worldwide per year, more than 95% of which occur in Asia and Africa. It is present in more than 150 countries and territories of all continents except Antarctica and some remote islands. There are more than 3 billion people living in regions of the world where it occurs. India has the highest rate of human rabies in the world, primarily because of stray dogs, whose number has greatly increased since a 2001 law forbade the killing of dogs. The people most at risk live in rural areas where human vaccines and immunoglobulin are not readily available or accessible.
Distribution of risk levels for humans contracting rabies, worldwide.
Signs and Symptoms
The incubation period
The incubation period is the time it takes for symptoms to develop after a person is infected with the virus. The incubation period for rabies is usually two to 12 weeks, although it can be as short as four days. It would be highly unusual for the incubation period to last for more than a year.
The closer the site of infection is to your brain, the shorter the incubation period. For example, a bite to your face, head or neck will have a shorter incubation period than a bite to your arm or leg. The length of the incubation period is important because it is the only period in which treatment can be successful.
Initial symptoms
The initial symptoms of rabies are often vague, and it can be easy to mistake them for other less serious types of infection. They include:
- High temperature of 100.4°F or above
- Chills
- Fatigue (extreme tiredness)
- Problems sleeping
- Lack of appetite
- Headache
- Irritability
- Anxiety
- Sore throat
- Vomiting
- Around half of people will also experience pain and a
tingling sensation at the site of the infection.
Advanced symptoms
Initial symptoms of rabies last for two to 10 days before more severe symptoms start to develop. There are two types of advanced rabies:
- Furious rabies, which accounts for four out of five cases
- Dumb or paralytic rabies, which accounts for the remainder of cases
Furious rabies
Furious rabies is characterised by episodes of increasingly odd and hyperactive behaviour, separated by periods of relative calm. During these episodes a person may have some or all of the following signs and symptoms:
- Aggressive behaviour, such as thrashing out or biting
- Agitation
- Hallucinations
- Delusions
- Excessive production of saliva
- High fever
- Excessive sweating
- Hair on their skin stands up
- In men, a sustained erection
Hydrophobia
People with furious rabies will also develop hydrophobia (a fear of water). This initially begins as a pain in the throat or difficulty swallowing. On attempting to swallow, the muscles in the throat go into a brief spasm that lasts for a few seconds. Subsequently the sight, sound or even the mention of water (or any other liquid) can trigger further spasms. There will also be fear of bright light (photophobia) and fear of breezes (aerophobia).
A few days after these symptoms develop, the affected person will fall into a coma and die, usually as a result of heart or lung failure.
Dumb or paralytic rabies
Dumb rabies, sometimes called paralytic rabies, is characterised by muscle weakness, loss of sensation and paralysis (inability to move one or more muscles). This usually begins in the hands and feet before spreading throughout the body.
Hydrophobia is unusual in cases of dumb rabies, although muscles may go into spasm. As with furious rabies, someone with dumb rabies will fall into a coma and eventually die from heart or lung failure.
Transmission
Rabies is common among wild animals in the United States. Bats, raccoons, skunks and foxes account for almost all reported cases (98% in 2009). Rabid bats are found in all 48 contiguous states. Other reservoirs are more limited geographically.
Worldwide
In developing countries, dogs account for the vast majority of human infections.
Treatment
A person exposed to rabies should ideally be treated within 12 hours of the exposure and definitely within 48 hours for the best outcome.
Post exposure prophylaxis (PEP) is critical to administer to any individual suspected of having been inoculated with the rabies virus. There are two primary components to PEP.
First, the bite wound, or suspected point of entry, must be thoroughly cleaned using soap and water for approximately five minutes, as soon as possible after exposure. This can help to reduce the number of virus particles that can gain entry into cells. Povidone iodine or alcohol is then recommended to reduce the virus further.
Second, vaccination must be provided as soon as possible following exposure. Rabies is one of the very few infections for which effective immunization can be administered after the exposure. This is due to the extended period of time required for the virus particles to reach the CNS and initiate pathogenesis. As such, PEP can be administered during the incubation period to effectively block pathogenesis.
It is critical to begin PEP as soon as possible following the exposure. In addition, the number of virions introduced to the infected individual as well as the site of introduction are important determinants of the duration of the incubation period. For example, individuals with multiple or severe bite wounds will typically have a larger inoculum, and those with bites on the hands, face, neck, or head will have a shorter distance for virions to travel before reaching the CNS. In either scenario, the incubation period can be reduced substantially. Children are also at greater risk because they typically experience bites on the face and head more frequently than adults.
A course of tissue culture vaccine should be administered, however it takes 1 to 2 weeks to mount an adequate humoral immune response. As such, the necessary antibodies may not be available in time for individuals with short incubation periods. Therefore, in addition to the tissue culture vaccine, passive immunity is relied on by administering antirabies immunoglobulin (RIG) in and around all bite wounds. The passive antibodies must be injected at the wound sites, not intramuscularly at some site distal to the wounds.
PEP is very expensive and often not available at all, in those areas of the world with high endemicity of rabies in dogs, particularly South and Southeast Asia and Africa. Thus, even if a rabies exposure is well documented and identified prior to the onset of symptoms, often supplies are inadequate to administer complete and effective PEP.
Prognosis
People who are treated early and appropriately when exposed to rabies have an excellent prognosis. No one who has begun treatment within 48 hours of exposure and has followed it appropriately has ever developed a fatal case of rabies in the U.S.
Untreated or inappropriately treated rabies is almost always fatal, death usually occurs in about seven days from respiratory failure after the more severe rabies symptoms develop. Treatment is supportive to limit the patient's pain, suffering, harm to the caregivers and self, and exposure of saliva to other humans. Barrier precautions (for example, gloves, gowns, and mask) are usually recommended for caregivers.
Signs of rabies in animals
After coming in contact with the virus, the bitten animal may go through one or all of several stages.
Animals may develop the paralytic (dumb) phase either after the prodromal or furious stage. The paralytic phase usually develops within 2 to 4 days after the first signs are noted. Nerves affecting the head and throat are the first to be involved and animals may begin to salivate as a result of their inability to swallow. Deep labored breathing and a dropped jaw may result as the diaphragm and facial muscles become increasingly paralyzed. Animals may make a choking sound and many owners think that there is something lodged in the dog's throat. The animal will get weaker and eventually go into respiratory failure and die.
Vaccination is the best way to prevent infection and properly vaccinated animals stand very little chance of contracting the disease. While rabies vaccination for dogs is mandatory for all states, it is estimated that up to half of all dogs are not vaccinated. Some communities are also requiring cats to be vaccinated, which is very important because there are currently more cases of cat rabies than dog rabies. Some people estimate that less than ten percent of the cat population is vaccinated thus leading to the high incidence of rabies in cats.
Wild
High-risk animal contacts for transmission of rabies are bats, raccoons, fox, skunks, and feral cats. Lower-risk animals are dogs, cats, coyote, deer, bear, horses, cattle, pigs, and other non-rodent wild animal species. The disease is almost never contracted from squirrels, rats, mice, or rabbits.
Readers should note that drooling saliva is not always present in wild or domestic animals with rabies. Any animal (domestic or wild) that acts strangely (for example, unusually aggressive or docile, unusual gait, has seizure-like activity) should be suspected of having rabies. Animals that are active at night (for example, raccoons, skunks and bats) may become active during the day; this daytime activity may be a sign of a rabies-infected animal.
In many cases, the infected animal is exceptionally aggressive, may attack without provocation, and exhibits otherwise uncharacteristic behavior.


